You Have Got Fallen Arches?
Overview

Fallen arches, the medical term for flat feet, are simply feet that do not arch in the middle. Such feet lay flat with the whole of the sole on the ground. All children are born with flat feet, but as they grow the feet normally develop an arch so that by the age of ten almost all children have arched feet. Occasionally a child will not develop properly arched feet. This may be due to a bone malformation present at birth, or abnormalities in ligaments within the feet or legs that cause the child's weight to be unevenly distributed.
Causes
There are a number of different causes that can lead to flat feet or fallen arches. These include, birth defects, while technically not a defect as such, flat feet can be a normal finding in patients from birth. However, a condition called tarsal coalition may occur where some of the bones in the foot are fused together resulting in a flatfoot. Inflammation or damage of the posterior tibial tendon. This tendon forms the end of a muscle that connects the lower leg to the foot, winding around the ankle and attaching to the inner aspect where the arch is normally present. The main role of the posterior tibial tendon is to invert the foot and maintain the arch height throughout the gait cycle. Torn muscles of the leg and foot can cause flat feet. Problems with the nerve supply to the muscles can result in reduction in tone and fallen arches. Fracture dislocation of the bones in the foot. Severe arthritis. While these are the common causes that can result in fallen arches and flat feet, it is important to recognise that there are certain risk factors that can also lead to this condition. These include advancing age, diabetes mellitus, high blood pressure, obesity and pregnancy.
Symptoms
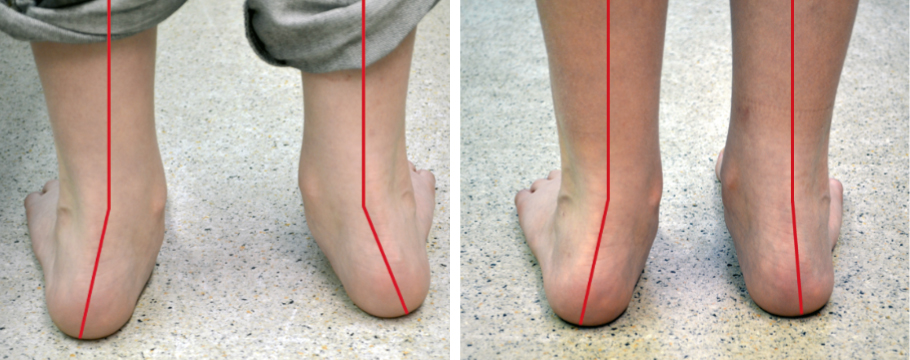
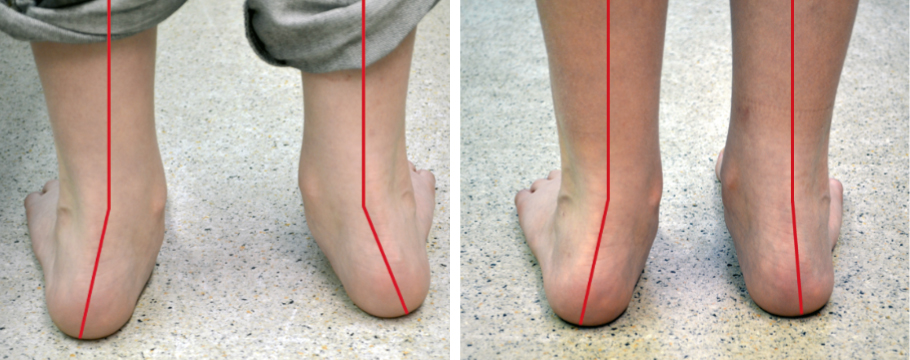
Most people do not exhibit any symptoms of flat feet, but if the condition is due to an underlying problem, symptoms can include foot pain, mainly in the arch or heel areas, difficulty standing on tiptoes, swelling that occurs on the inside of the ankle, pain in the calf, knee, hip, or lower leg area, both feet lie flat on the ground with no gap, Shoes may not fit properly, heel may tilt away from the midline of the body more than usual, absence of foot arch when standing. If you are experiencing these symptoms and have flat feet, you should consider seeing your doctor or a podiatrist immediately for an examination.
Diagnosis
It is important for people with foot pain to know if they have flat feet. The following tests can help you determine your arch type. When you get out of a swimming pool, look at your footprint on the concrete. The front of the foot will be joined to the heel by a strip. If your foot is flat, then the strip is the same width as the front of the foot, creating a footprint that looks like a stretched out pancake. With a normal arch, the strip is about half the width of the front of the foot. If you have a high arch, only a thin strip connects the front of the foot with the heel. Put your shoes on a flat table and view them at eye level from behind. See if the sole is worn evenly. A flat foot will cause more wear on the inside of the sole, especially in the heel area. The shoe will easily rock side to side. A flat foot will also cause the upper part of the shoe to lean inward over the sole. Both shoes should wear about the same way. If you have pain in one foot, you should make sure you don't have a fallen arch on that side. There are two good tests you can perform at home to detect this problem. Place your fingertips on a wall that you are directly facing and stand on your tiptoes on one foot. If you can't do it, a fallen arch may be the culprit. Stand with your feet parallel. Have someone stand in back of you and look at your feet from behind. You can also do it yourself if you stand with your back to a mirror. Normally, only the pinky toe is visible from behind. If one foot is flatter than the other, the 4th and sometimes the 3rd toe on that foot can also be seen.
pes cavus
Non Surgical Treatment
In rare cases, surgery may be needed if a child has flat feet caused by a problem they're born with (a congenital abnormality). The foot may need to be straightened or the bones may need to be separated if they're fused together. Painkillers and insoles are the first treatment options for flat feet that are caused by a joint problem, such as arthritis or a torn tendon. However, surgery may be recommended if the injury or condition is severely affecting your feet. Where flat feet are caused by a condition that affects the nervous system, special shoes, insoles, or supportive foot or leg braces may be needed. Again, in severe cases, an operation may be needed to straighten the feet.
Surgical Treatment
In cases of flat feet that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required and in some advanced cases, surgery may be the only option. Your foot and ankle surgeon will determine the best approach for you.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.

Fallen arches, the medical term for flat feet, are simply feet that do not arch in the middle. Such feet lay flat with the whole of the sole on the ground. All children are born with flat feet, but as they grow the feet normally develop an arch so that by the age of ten almost all children have arched feet. Occasionally a child will not develop properly arched feet. This may be due to a bone malformation present at birth, or abnormalities in ligaments within the feet or legs that cause the child's weight to be unevenly distributed.
Causes
There are a number of different causes that can lead to flat feet or fallen arches. These include, birth defects, while technically not a defect as such, flat feet can be a normal finding in patients from birth. However, a condition called tarsal coalition may occur where some of the bones in the foot are fused together resulting in a flatfoot. Inflammation or damage of the posterior tibial tendon. This tendon forms the end of a muscle that connects the lower leg to the foot, winding around the ankle and attaching to the inner aspect where the arch is normally present. The main role of the posterior tibial tendon is to invert the foot and maintain the arch height throughout the gait cycle. Torn muscles of the leg and foot can cause flat feet. Problems with the nerve supply to the muscles can result in reduction in tone and fallen arches. Fracture dislocation of the bones in the foot. Severe arthritis. While these are the common causes that can result in fallen arches and flat feet, it is important to recognise that there are certain risk factors that can also lead to this condition. These include advancing age, diabetes mellitus, high blood pressure, obesity and pregnancy.
Symptoms
Most people do not exhibit any symptoms of flat feet, but if the condition is due to an underlying problem, symptoms can include foot pain, mainly in the arch or heel areas, difficulty standing on tiptoes, swelling that occurs on the inside of the ankle, pain in the calf, knee, hip, or lower leg area, both feet lie flat on the ground with no gap, Shoes may not fit properly, heel may tilt away from the midline of the body more than usual, absence of foot arch when standing. If you are experiencing these symptoms and have flat feet, you should consider seeing your doctor or a podiatrist immediately for an examination.
Diagnosis
It is important for people with foot pain to know if they have flat feet. The following tests can help you determine your arch type. When you get out of a swimming pool, look at your footprint on the concrete. The front of the foot will be joined to the heel by a strip. If your foot is flat, then the strip is the same width as the front of the foot, creating a footprint that looks like a stretched out pancake. With a normal arch, the strip is about half the width of the front of the foot. If you have a high arch, only a thin strip connects the front of the foot with the heel. Put your shoes on a flat table and view them at eye level from behind. See if the sole is worn evenly. A flat foot will cause more wear on the inside of the sole, especially in the heel area. The shoe will easily rock side to side. A flat foot will also cause the upper part of the shoe to lean inward over the sole. Both shoes should wear about the same way. If you have pain in one foot, you should make sure you don't have a fallen arch on that side. There are two good tests you can perform at home to detect this problem. Place your fingertips on a wall that you are directly facing and stand on your tiptoes on one foot. If you can't do it, a fallen arch may be the culprit. Stand with your feet parallel. Have someone stand in back of you and look at your feet from behind. You can also do it yourself if you stand with your back to a mirror. Normally, only the pinky toe is visible from behind. If one foot is flatter than the other, the 4th and sometimes the 3rd toe on that foot can also be seen.
pes cavus
Non Surgical Treatment
In rare cases, surgery may be needed if a child has flat feet caused by a problem they're born with (a congenital abnormality). The foot may need to be straightened or the bones may need to be separated if they're fused together. Painkillers and insoles are the first treatment options for flat feet that are caused by a joint problem, such as arthritis or a torn tendon. However, surgery may be recommended if the injury or condition is severely affecting your feet. Where flat feet are caused by a condition that affects the nervous system, special shoes, insoles, or supportive foot or leg braces may be needed. Again, in severe cases, an operation may be needed to straighten the feet.
Surgical Treatment
In cases of flat feet that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required and in some advanced cases, surgery may be the only option. Your foot and ankle surgeon will determine the best approach for you.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
Leg Length Discrepancy Shoe Wear
Overview
Leg length discrepancy (LLD) affects about 70% of the general population, and can be either structural - when the difference occurs in bone structures - or functional, because of mechanical changes at the lower limbs. The discrepancy can be also classified by its magnitude into mild, intermediate, or severe. Mild LLD has been particularly associated with stress fracture, low back pain and osteoarthritis, and when the discrepancy occurs in subjects whose mechanical loads are increased by their professional, daily or recreational activities, these orthopaedic changes may appear early and severely. The aim of this study was to analyze and compare ground reaction force (GRF) during gait in runners with and without mild LLD. Results showed that subjects with mild LLD of 0.5 to 2.0 cm presented higher values of minimum vertical GRF (0.57 ? 0.07 BW) at the shorter limb compared to the longer limb (0.56 ? 0.08 BW) Therefore, subjects with mild LLD adopt compensatory mechanisms that cause additional overloads to the musculoskeletal system in order to promote a symmetrical gait pattern as showed by the values of absolute symmetric index of vertical and horizontal GRF variables.
Causes
Limb-length conditions can result from congenital disorders of the bones, muscles or joints, disuse or overuse of the bones, muscles or joints caused by illness or disease, diseases, such as bone cancer, Issues of the spine, shoulder or hip, traumatic injuries, such as severe fractures that damage growth plates.
Symptoms
The patient/athlete may present with an altered gait (such as limping) and/or scoliosis and/or low back pain. Lower extremity disorders are possibly associated with LLD, some of these are increased hip pain and degeneration (especially involving the long leg). Increased risk of: knee injury, ITB syndrome, pronation and plantar fascitis, asymmetrical strength in lower extremity. Increased disc or vertebral degeneration. Symptoms vary between patients, some patients may complain of just headaches.
Diagnosis
Asymmetry is a clue that a LLD is present. The center of gravity will shift to the short limb side and patients will try to compensate, displaying indications such as pelvic tilt, lumbar scoliosis, knee flexion, or unilateral foot pronation. Asking simple questions such as, "Do you favor one leg over the other?" or, "Do you find it uncomfortable to stand?" may also provide some valuable information. Performing a gait analysis will yield some clues as to how the patient compensates during ambulation. Using plantar pressure plates can indicate load pressure differences between the feet. It is helpful if the gait analysis can be video-recorded and played back in slow motion to catch the subtle aspects of movement.
Non Surgical Treatment
Whether or not treatment should be pursued depends on the amount of discrepancy. In general, no treatment (other than a heel life, if desired) should be considered for discrepancies under two centimeters. If the discrepancy measures between two and five centimeters, one might consider a procedure to equalize leg length. Usually, this would involve closure of the growth plate on the long side, thereby allowing the short side to catch up; shortening the long leg; or possibly lengthening the short leg.

how to become tall in one day
Surgical Treatment
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.
Leg length discrepancy (LLD) affects about 70% of the general population, and can be either structural - when the difference occurs in bone structures - or functional, because of mechanical changes at the lower limbs. The discrepancy can be also classified by its magnitude into mild, intermediate, or severe. Mild LLD has been particularly associated with stress fracture, low back pain and osteoarthritis, and when the discrepancy occurs in subjects whose mechanical loads are increased by their professional, daily or recreational activities, these orthopaedic changes may appear early and severely. The aim of this study was to analyze and compare ground reaction force (GRF) during gait in runners with and without mild LLD. Results showed that subjects with mild LLD of 0.5 to 2.0 cm presented higher values of minimum vertical GRF (0.57 ? 0.07 BW) at the shorter limb compared to the longer limb (0.56 ? 0.08 BW) Therefore, subjects with mild LLD adopt compensatory mechanisms that cause additional overloads to the musculoskeletal system in order to promote a symmetrical gait pattern as showed by the values of absolute symmetric index of vertical and horizontal GRF variables.

Causes
Limb-length conditions can result from congenital disorders of the bones, muscles or joints, disuse or overuse of the bones, muscles or joints caused by illness or disease, diseases, such as bone cancer, Issues of the spine, shoulder or hip, traumatic injuries, such as severe fractures that damage growth plates.
Symptoms
The patient/athlete may present with an altered gait (such as limping) and/or scoliosis and/or low back pain. Lower extremity disorders are possibly associated with LLD, some of these are increased hip pain and degeneration (especially involving the long leg). Increased risk of: knee injury, ITB syndrome, pronation and plantar fascitis, asymmetrical strength in lower extremity. Increased disc or vertebral degeneration. Symptoms vary between patients, some patients may complain of just headaches.
Diagnosis
Asymmetry is a clue that a LLD is present. The center of gravity will shift to the short limb side and patients will try to compensate, displaying indications such as pelvic tilt, lumbar scoliosis, knee flexion, or unilateral foot pronation. Asking simple questions such as, "Do you favor one leg over the other?" or, "Do you find it uncomfortable to stand?" may also provide some valuable information. Performing a gait analysis will yield some clues as to how the patient compensates during ambulation. Using plantar pressure plates can indicate load pressure differences between the feet. It is helpful if the gait analysis can be video-recorded and played back in slow motion to catch the subtle aspects of movement.
Non Surgical Treatment
Whether or not treatment should be pursued depends on the amount of discrepancy. In general, no treatment (other than a heel life, if desired) should be considered for discrepancies under two centimeters. If the discrepancy measures between two and five centimeters, one might consider a procedure to equalize leg length. Usually, this would involve closure of the growth plate on the long side, thereby allowing the short side to catch up; shortening the long leg; or possibly lengthening the short leg.

how to become tall in one day
Surgical Treatment
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.
Combating Mortons Neuroma
Overview
 Morton neuromas are focal areas of symptomatic perineural fibrosis around a plantar digital nerve of the foot. The abnormality is non-neoplastic and does not represent a true neuroma. It may more correctly be known as Morton?s metatarsalgia. The condition is thought to be due to chronic entrapment of the nerve by the intermetatarsal ligament. It most often occurs in middle-aged individuals and is many times more common in women than men. Approximately 30% of asymptomatic middle-aged persons have the radiological pathologic findings of a Morton?s neuroma.
Morton neuromas are focal areas of symptomatic perineural fibrosis around a plantar digital nerve of the foot. The abnormality is non-neoplastic and does not represent a true neuroma. It may more correctly be known as Morton?s metatarsalgia. The condition is thought to be due to chronic entrapment of the nerve by the intermetatarsal ligament. It most often occurs in middle-aged individuals and is many times more common in women than men. Approximately 30% of asymptomatic middle-aged persons have the radiological pathologic findings of a Morton?s neuroma.
Causes
Morton's neuroma is an inflammation caused by a buildup of fibrous tissue on the outer coating of nerves. This fibrous buildup is a reaction to the irritation resulting from nearby bones and ligaments rubbing against the nerves. Irritation can be caused by Wearing shoes that are too tight. Wearing shoes that place the foot in an awkward position, such as high heels. A foot that is mechanically unstable. Repetitive trauma to the foot such as from sports activities like tennis, basketball, and running. Trauma to the foot caused by an injury such as a sprain or fracture. It is unusual for more than one Morton's neuroma to occur on one foot at the same time. It is rare for Morton's neuroma to occur on both feet at the same time.
Symptoms
Episodes of pain are intermittent. Patients may experience 2 attacks in a week and then none for a year. Recurrences are variable and tend to become more frequent. Between attacks, no symptoms or physical signs occur. Two neuromas coexist on the same foot about 2-3% of the time. Other diagnoses should be considered when 2 or more areas of tenderness are present.
Diagnosis
Your health care provider can usually diagnose this problem by examining your foot. A foot x-ray may be done to rule out bone problems. MRI or high-resolution ultrasound can successfully diagnose Morton's neuroma. Nerve testing (electromyography) cannot diagnose Morton's neuroma, but may be used to rule out conditions that cause similar symptoms. Blood tests may be done to check for inflammation-related conditions, including certain forms of arthritis.
Non Surgical Treatment
Conservative treatment for Morton?s neuroma involves footwear that allows your forefoot to spread. High-heeled shoes cause neuromas by squeezing and stretching your involved intermetatarsal nerve across the ball of your foot and should be avoided as often as possible. A shoe that possesses any toe spring will also place more stress on your foot nerves and increase your likelihood of developing a neuroma. Test shoes before you buy them to see if they are appropriate for your feet. Select shoes that have a removable liner or insole, and stand on the liner, noting the position of your foot. If your foot is wider than your liner, that shoe will irritate your neuroma by squeezing your metatarsal bones together.
Surgical Treatment
Surgery to excise the neuroma is usually performed under general anaesthetic in a day surgery facility. After surgery you will have to keep your foot dry for two weeks. Generally neuroma surgery allows for early weight bearing and protection in some type of post op shoe gear. Some neuromas may reoccur, but this is rare. Most studies on patient satisfaction after neuroma surgery show approximately 90% reduction of pain and about 85% of all patients rated the overall satisfaction with the results as excellent or good.
 Morton neuromas are focal areas of symptomatic perineural fibrosis around a plantar digital nerve of the foot. The abnormality is non-neoplastic and does not represent a true neuroma. It may more correctly be known as Morton?s metatarsalgia. The condition is thought to be due to chronic entrapment of the nerve by the intermetatarsal ligament. It most often occurs in middle-aged individuals and is many times more common in women than men. Approximately 30% of asymptomatic middle-aged persons have the radiological pathologic findings of a Morton?s neuroma.
Morton neuromas are focal areas of symptomatic perineural fibrosis around a plantar digital nerve of the foot. The abnormality is non-neoplastic and does not represent a true neuroma. It may more correctly be known as Morton?s metatarsalgia. The condition is thought to be due to chronic entrapment of the nerve by the intermetatarsal ligament. It most often occurs in middle-aged individuals and is many times more common in women than men. Approximately 30% of asymptomatic middle-aged persons have the radiological pathologic findings of a Morton?s neuroma.Causes
Morton's neuroma is an inflammation caused by a buildup of fibrous tissue on the outer coating of nerves. This fibrous buildup is a reaction to the irritation resulting from nearby bones and ligaments rubbing against the nerves. Irritation can be caused by Wearing shoes that are too tight. Wearing shoes that place the foot in an awkward position, such as high heels. A foot that is mechanically unstable. Repetitive trauma to the foot such as from sports activities like tennis, basketball, and running. Trauma to the foot caused by an injury such as a sprain or fracture. It is unusual for more than one Morton's neuroma to occur on one foot at the same time. It is rare for Morton's neuroma to occur on both feet at the same time.
Symptoms
Episodes of pain are intermittent. Patients may experience 2 attacks in a week and then none for a year. Recurrences are variable and tend to become more frequent. Between attacks, no symptoms or physical signs occur. Two neuromas coexist on the same foot about 2-3% of the time. Other diagnoses should be considered when 2 or more areas of tenderness are present.
Diagnosis
Your health care provider can usually diagnose this problem by examining your foot. A foot x-ray may be done to rule out bone problems. MRI or high-resolution ultrasound can successfully diagnose Morton's neuroma. Nerve testing (electromyography) cannot diagnose Morton's neuroma, but may be used to rule out conditions that cause similar symptoms. Blood tests may be done to check for inflammation-related conditions, including certain forms of arthritis.
Non Surgical Treatment
Conservative treatment for Morton?s neuroma involves footwear that allows your forefoot to spread. High-heeled shoes cause neuromas by squeezing and stretching your involved intermetatarsal nerve across the ball of your foot and should be avoided as often as possible. A shoe that possesses any toe spring will also place more stress on your foot nerves and increase your likelihood of developing a neuroma. Test shoes before you buy them to see if they are appropriate for your feet. Select shoes that have a removable liner or insole, and stand on the liner, noting the position of your foot. If your foot is wider than your liner, that shoe will irritate your neuroma by squeezing your metatarsal bones together.

Surgical Treatment
Surgery to excise the neuroma is usually performed under general anaesthetic in a day surgery facility. After surgery you will have to keep your foot dry for two weeks. Generally neuroma surgery allows for early weight bearing and protection in some type of post op shoe gear. Some neuromas may reoccur, but this is rare. Most studies on patient satisfaction after neuroma surgery show approximately 90% reduction of pain and about 85% of all patients rated the overall satisfaction with the results as excellent or good.
Why Shoe Lifts Are The Ideal Solution To Leg Length Difference
There are actually two unique variations of leg length discrepancies, congenital and acquired. Congenital implies you are born with it. One leg is anatomically shorter than the other. Through developmental phases of aging, the brain senses the stride pattern and identifies some variation. The entire body typically adapts by dipping one shoulder to the "short" side. A difference of less than a quarter inch isn't really irregular, require Shoe Lifts to compensate and usually doesn't have a profound effect over a lifetime.

Leg length inequality goes largely undiagnosed on a daily basis, however this problem is very easily remedied, and can reduce many incidents of back discomfort.
Therapy for leg length inequality usually involves Shoe Lifts. These are generally affordable, commonly being under twenty dollars, in comparison to a custom orthotic of $200 or more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Lumbar pain is the most prevalent health problem affecting men and women today. Over 80 million people have problems with back pain at some stage in their life. It is a problem which costs businesses vast amounts of money each year on account of lost time and production. Fresh and better treatment methods are always sought after in the hope of lowering economical impact this condition causes.

Men and women from all corners of the earth suffer the pain of foot ache due to leg length discrepancy. In these situations Shoe Lifts can be of worthwhile. The lifts are capable of easing any discomfort in the feet. Shoe Lifts are recommended by many specialist orthopaedic physicians.
So as to support the body in a well-balanced fashion, the feet have got a very important function to play. In spite of that, it is sometimes the most neglected zone of the body. Some people have flat-feet which means there is unequal force exerted on the feet. This causes other body parts such as knees, ankles and backs to be affected too. Shoe Lifts make sure that the right posture and balance are restored.

Leg length inequality goes largely undiagnosed on a daily basis, however this problem is very easily remedied, and can reduce many incidents of back discomfort.
Therapy for leg length inequality usually involves Shoe Lifts. These are generally affordable, commonly being under twenty dollars, in comparison to a custom orthotic of $200 or more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Lumbar pain is the most prevalent health problem affecting men and women today. Over 80 million people have problems with back pain at some stage in their life. It is a problem which costs businesses vast amounts of money each year on account of lost time and production. Fresh and better treatment methods are always sought after in the hope of lowering economical impact this condition causes.

Men and women from all corners of the earth suffer the pain of foot ache due to leg length discrepancy. In these situations Shoe Lifts can be of worthwhile. The lifts are capable of easing any discomfort in the feet. Shoe Lifts are recommended by many specialist orthopaedic physicians.
So as to support the body in a well-balanced fashion, the feet have got a very important function to play. In spite of that, it is sometimes the most neglected zone of the body. Some people have flat-feet which means there is unequal force exerted on the feet. This causes other body parts such as knees, ankles and backs to be affected too. Shoe Lifts make sure that the right posture and balance are restored.
Tips To Identify Heel Spur

Overview
Heel spurs refer to the abnormal accumulation of calcium deposits on the heel of the foot. Vigorous, repetitive movements often result in the formation of heel spurs, but inflammatory diseases (e.g., arthritis) may also increase the occurrence of painful heel spurs. Treatments that have proven to be effective for heel spurs include injections that contain a combination of steroids and anesthesia as well as radiofrequency ablation. However, a bone spur that begins to protrude excessively may need to be removed through surgery.
Causes
You are more likely to develop plantar fasciitis and heel spurs if you are Active. Sports that place excessive stress on the heel bone and attached tissue, especially if you have tight calf muscles or a stiff ankle from a previous ankle sprain, which limits ankle movement eg. running, ballet dancing and aerobics. Overweight. Carrying around extra weight increases the strain and stress on your plantar fascia. Pregnant. The weight gain and swelling associated with pregnancy can cause ligaments to become more relaxed, which can lead to mechanical problems and inflammation. On your feet. Having a job that requires a lot of walking or standing on hard surfaces ie factory workers, teachers and waitresses. Flat Feet or High Foot Arches. Changes in the arch of your foot changes the shock absorption ability and can stretch and strain the plantar fascia, which then has to absorb the additional force. Middle-Aged or Older. With ageing the arch of your foot may begin to sag - putting extra stress on the plantar fascia. Wearing shoes with poor support. Weak Foot Arch Muscles. Muscle fatigue allows your plantar fascia to overstress and cause injury. Arthritis. Some types of arthritis can cause inflammation in the tendons in the bottom of your foot, which may lead to plantar fasciitis. Diabetes. Although doctors don't know why, plantar fasciitis occurs more often in people with diabetes.

Symptoms
Heel spurs result in a jabbing or aching sensation on or under the heel bone. The pain is often worst when you first arise in the morning and get to your feet. You may also experience pain when standing up after prolonged periods of sitting, such as work sessions at a desk or car rides. The discomfort may lessen after you spend several minutes walking, only to return later. Heel spurs can cause intermittent or chronic pain.
Diagnosis
Heel spurs and plantar fasciitis is usually diagnosed by your physiotherapist or sports doctor based on your symptoms, history and clinical examination. After confirming your heel spur or plantar fasciitis they will investigate WHY you are likely to be predisposed to heel spurs and develop a treatment plan to decrease your chance of future bouts. X-rays will show calcification or bone within the plantar fascia or at its insertion into the calcaneus. This is known as a calcaneal or heel spur. Ultrasound scans and MRI are used to identify any plantar fasciitis tears, inflammation or calcification. Pathology tests may identify spondyloarthritis, which can cause symptoms similar to plantar fasciitis.
Non Surgical Treatment
Only in rare cases do the symptoms of heel spurs fail to be resolved through conservative treatment. Conservative treatment, although not 100% effective, is successful in most cases and should be given ample time to work. In many cases, conservative methods should be utilized as long as a year depending on the rate at which your body responds to the treatment. When treatment is unsuccessful, surgery may be considered. A common surgical procedure for this condition is plantar fascia release surgery. In this procedure, the tension of the plantar fascia ligament is released, lessening tension in the heel and helping to prevent damage.
Surgical Treatment
Usually, heel spurs are curable with conservative treatment. If not, heel spurs are curable with surgery, although there is the possibility of them growing back. About 10% of those who continue to see a physician for plantar fascitis have it for more than a year. If there is limited success after approximately one year of conservative treatment, patients are often advised to have surgery.
Prevention
To prevent this condition, wearing properly fitted shoes with good arch support is very important. If a person is overweight, weight loss can help diminish stress on the feet and help prevent foot problems. For those who exercise frequently and intensely, proper stretching is always necessary, especially when there is an increase in activities or a change in running technique. It is not recommended to attempt to work through the pain, as this can change a mild case of heel spurs and plantar fascitis into a long-lasting and painful episode of the condition.
The Causes Of Inferior Calcaneal Spur

Overview
Bone spurs (retrocalcaneal spur, or exostosis) can develop not only on the back of the heel, but also on the toes, mainly around the fifth (small) toe. Most often, they occur next to the toenail on the outside of the toe; on the inside of the toe near the tip, where the fifth toe presses against the fourth toe; and on the inside of the base of the toe. Bone spurs can also occur on the sides of the toes. This is usually due to wearing shoes that are too tight in the toe box, which causes the toes to press against each other. Bone spurs may also develop in the arch area of the top of the foot; this area becomes painful when you tie your shoelaces tightly or exert other pressure on that part of the foot. Formation of spurs in this area is often associated with arthritis.
Causes
An individual with the lower legs angulating inward, a condition called genu valgum or "knock knees," can have a tendency toward excessive pronation. As a result, this too can lead to a fallen arch resulting in plantar fascitis and heel spurs. Women tend to have more genu valgum than men do. Heel spurs can also result from an abnormally high arch. Other factors leading to heel spurs include a sudden increase in daily activities, an increase in weight, or a change of shoes. Dramatic increase in training intensity or duration may cause plantar fascitis. Shoes that are too flexible in the middle of the arch or shoes that bend before the toe joints will cause an increase in tension in the plantar fascia and possibly lead to heel spurs.

Symptoms
Symptoms of heel spur syndrome often include pain early in the morning or after rest, as you take the first few steps. It may also include severe pain after standing or walking long hours, especially on hard cement floors. Usually more pain exist while wearing a very flat soled shoe. A higher heel may actually relieve the pain as an arch is created. The pain is usually sharp, but can also be a dull ache. The pain may only be at the bottom of the heel, or may also travel along the arch of the foot.
Diagnosis
The proper diagnosis of a heel spur often requires an X-ray. To make this process as convenient for his patients as possible, most clinics have an on-site digital X-ray and diagnostic ultrasound machines. This can make it unnecessary for patients to visit diagnostic imaging centers, allowing patients to receive more expedient treatment.
Non Surgical Treatment
In case of heel spurs rest is most important. Active sports, running, long walks etc should be avoided to start with. If you?re in a job that requires a lot of standing, take a few days off work. Rest (or reduced activity) is essential to allow the inflammation from becoming aggrevated. Furthermore, you can use ice packs (placed on the heel for 5-10 minutes) to ?cool down? the inflamed area. You may take anti-inflammatory medication or apply a topical inflammatory (i.e. a cream) to help reduce inflammation. In addition, there are some simple exercises that should be done daily to help relieve heel spur pain.
Surgical Treatment
When chronic heel pain fails to respond to conservative treatment, surgical treatment may be necessary. Heel surgery can provide pain relief and restore mobility. The type of procedure used is based on examination and usually consists of releasing the excessive tightness of the plantar fascia, called a plantar fascia release. The procedure may also include removal of heel spurs.
Bursa Foot Surgery Recovery
Overview
Between the heel bone and the plantar fascia is a small fluid filled sac that is called the plantar (bottom of) calcaneal (heel bone) bursa. The plantar calcaneal bursa?s job is to allow the plantar fascia to glide easily over the heel bone without irritation. If this becomes inflamed and irritated a plantar calcaneal bursitis occurs which can be extremely painful and disabling forcing the athlete to stop training.
Causes
For the most part, it is a genetic condition. You develop it by inheriting a foot type that is prone to the mechanical irritation that leads to the problem. If you have this particular foot type and wear shoes that rub and irritate the back of the heel bone (calcaneus) where the Achilles tendon attaches, then you are even more likely to develop this type of bursitis. The contributing factors include a supinated foot type, a heel bone with a prominence (or pointed shape that stick out toward the tendon) at the back, a tight Achilles tendon (referred to as Equinus by doctors), and a high arch. All of these factors simply make it more likely that the back of the heel will press against the shoe and rub. As the tendon gets rubbed the wrong way, the bursa starts to develop and fill with fluid. This response is really your body's way of protecting the tendon from damage, but it backfires. The friction from all that rubbing causes the bursa to become inflamed and swell. This causes the bump to become red, hot and stick out even further. Much like a sore thumb, it then gets irritated by even the softest shoes.
Symptoms
Pain and tenderness usually develop slowly over time. Applying pressure to the back of the heel can cause pain. Wearing shoes may become uncomfortable. The back of the heel may feel achy. Pain is exacerbated when the foot is pointed or flexed, because the swollen bursa can get squeezed. A person with retrocalcaneal bursitis may feel pain when standing on their toes. Fever or chills in addition to other bursitis symptoms can be a sign of septic bursitis. Though uncommon, septic retrocalcaneal bursitis is a serious condition, and patients should seek medical care to ensure the infection does not spread.
Diagnosis
Your health care provider will take a history to find out if you have symptoms of retrocalcaneal bursitis. Examining your ankle can find the location of the pain. The physician will look for tenderness and redness in the back of the heel. The pain may be worse when the doctor bends the ankle upward (dorsiflex). Or, the pain may be worse when you rise on your toes. You will not usually need imaging studies such as x-ray and MRI at first. If the first treatment does not improve the symptoms, your health care provider may recommend these tests. MRI may show inflammation.
Non Surgical Treatment
During the initial acute phase of the condition, patients should apply ice to the back of the heel for 15 to 20 minutes and follow the R.I.C.E.R regime. Avoid activities that cause pain. Gradual progressive stretching of the calf muscle and Achilles tendon is also advocated. Changing the footwear. Wearing an open-backed shoe may help relieve pressure on the affected region. For those whose symptoms were caused by a sudden change from wearing high-heeled shoes to flat shoes, the temporary use of footwear with a heel height in between may be helpful. Inserting a heel cup in the shoe may help to raise the inflamed region slightly above the shoe?s restricting heel counter and relieve the pain. It is advisable to also insert the heel cup into the other shoe to avoid any leg-leg discrepancies that can lead to other problems. Training frequency and intensity should be gradually progressed with adequate rest between trainings.
Surgical Treatment
Surgery is rarely done strictly for treatment of a bursitis. If any underlying cause is the reason, this may be addressed surgically. During surgery for other conditions, a bursa may be seen and removed surgically.
Between the heel bone and the plantar fascia is a small fluid filled sac that is called the plantar (bottom of) calcaneal (heel bone) bursa. The plantar calcaneal bursa?s job is to allow the plantar fascia to glide easily over the heel bone without irritation. If this becomes inflamed and irritated a plantar calcaneal bursitis occurs which can be extremely painful and disabling forcing the athlete to stop training.
Causes
For the most part, it is a genetic condition. You develop it by inheriting a foot type that is prone to the mechanical irritation that leads to the problem. If you have this particular foot type and wear shoes that rub and irritate the back of the heel bone (calcaneus) where the Achilles tendon attaches, then you are even more likely to develop this type of bursitis. The contributing factors include a supinated foot type, a heel bone with a prominence (or pointed shape that stick out toward the tendon) at the back, a tight Achilles tendon (referred to as Equinus by doctors), and a high arch. All of these factors simply make it more likely that the back of the heel will press against the shoe and rub. As the tendon gets rubbed the wrong way, the bursa starts to develop and fill with fluid. This response is really your body's way of protecting the tendon from damage, but it backfires. The friction from all that rubbing causes the bursa to become inflamed and swell. This causes the bump to become red, hot and stick out even further. Much like a sore thumb, it then gets irritated by even the softest shoes.
Symptoms
Pain and tenderness usually develop slowly over time. Applying pressure to the back of the heel can cause pain. Wearing shoes may become uncomfortable. The back of the heel may feel achy. Pain is exacerbated when the foot is pointed or flexed, because the swollen bursa can get squeezed. A person with retrocalcaneal bursitis may feel pain when standing on their toes. Fever or chills in addition to other bursitis symptoms can be a sign of septic bursitis. Though uncommon, septic retrocalcaneal bursitis is a serious condition, and patients should seek medical care to ensure the infection does not spread.
Diagnosis
Your health care provider will take a history to find out if you have symptoms of retrocalcaneal bursitis. Examining your ankle can find the location of the pain. The physician will look for tenderness and redness in the back of the heel. The pain may be worse when the doctor bends the ankle upward (dorsiflex). Or, the pain may be worse when you rise on your toes. You will not usually need imaging studies such as x-ray and MRI at first. If the first treatment does not improve the symptoms, your health care provider may recommend these tests. MRI may show inflammation.
Non Surgical Treatment
During the initial acute phase of the condition, patients should apply ice to the back of the heel for 15 to 20 minutes and follow the R.I.C.E.R regime. Avoid activities that cause pain. Gradual progressive stretching of the calf muscle and Achilles tendon is also advocated. Changing the footwear. Wearing an open-backed shoe may help relieve pressure on the affected region. For those whose symptoms were caused by a sudden change from wearing high-heeled shoes to flat shoes, the temporary use of footwear with a heel height in between may be helpful. Inserting a heel cup in the shoe may help to raise the inflamed region slightly above the shoe?s restricting heel counter and relieve the pain. It is advisable to also insert the heel cup into the other shoe to avoid any leg-leg discrepancies that can lead to other problems. Training frequency and intensity should be gradually progressed with adequate rest between trainings.
Surgical Treatment
Surgery is rarely done strictly for treatment of a bursitis. If any underlying cause is the reason, this may be addressed surgically. During surgery for other conditions, a bursa may be seen and removed surgically.