Do I Suffer From Overpronation
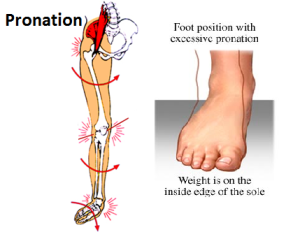
During initial contact or heel strike, the ankle rolls inward, causing excessive pronation or flattening of the foot. This action forces the big toe (instead of the ball of foot and all toes) to do all the work to push off the ground. When the ankle overpronates, this causes the tibia (shin bone) to rotate and the femur (thigh bone) to adduct (move toward the mid-line of the body), causing internal rotation or knee valgus (knock-kneed).

Causes
There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. Often people with flat feet do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
When standing, your heels lean inward. When standing, one or both of your knee caps turn inward. Conditions such as a flat feet or bunions may occur. You develop knee pain when you are active or involved in athletics. The knee pain slowly goes away when you rest. You abnormally wear out the soles and heels of your shoes very quickly.
Diagnosis
To easily get an idea of whether a person overpronates, look at the position and condition of certain structures in the feet and ankles when he/she stands still. When performing weight-bearing activities like walking or running, muscles and other soft tissue structures work to control gravity's effect and ground reaction forces to the joints. If the muscles of the leg, pelvis, and feet are working correctly, then the joints in these areas such as the knees, hips, and ankles will experience less stress. However, if the muscles and other soft tissues are not working efficiently, then structural changes and clues in the feet are visible and indicate habitual overpronation.
Non Surgical Treatment
Overpronation is a condition in which the foot rolls excessively down and inward. The arch may elongate and collapse (or ?fall?) and the heel will lean inward. Overpronation should not be confused with pronation. Pronation is a normal motion of the foot during weight bearing and allows the foot to absorb shock as it contacts the ground.
Prevention
Duck stance: Stand with your heels together and feet turned out. Tighten the buttock muscles, slightly tilt your pelvis forwards and try to rotate your legs outwards. You should feel your arches rising while you do this exercise.
Calf stretch:Stand facing a wall and place hands on it for support. Lean forwards until stretch is felt in the calves. Hold for 30 seconds. Bend at knees and hold for a further 30 seconds. Repeat 5 times.
Golf ball:While drawing your toes upwards towards your shins, roll a golf ball under the foot between 30 and 60 seconds. If you find a painful point, keep rolling the ball on that spot for 10 seconds.
Big toe push: Stand with your ankles in a neutral position (without rolling the foot inwards). Push down with your big toe but do not let the ankle roll inwards or the arch collapse. Hold for 5 seconds. Repeat 10 times. Build up to longer times and fewer repetitions.
Ankle strengthener: Place a ball between your foot and a wall. Sitting down and keeping your toes pointed upwards, press the outside of the foot against the ball, as though pushing it into the wall. Hold for 5 seconds and repeat 10 times.
Arch strengthener: Stand on one foot on the floor. The movements needed to remain balanced will strengthen the arch. When you are able to balance for 30 seconds, start doing this exercise using a wobble board.
Severs Disease The Facts
Severs disease or calcaneal apophysitis causes heel pain usually in growing children between age nine and fourteen. It occurs as a result of disturbance during the final development of the heel growth plate. During this time the achilles tendon is pulling strongly on the heel bone and this excessive force can cause inflammation and pain.
Causes
There is no specific known cause of Sever?s disease. However, there are several common factors associated with the condition including. Tight calf muscles. Pronated foot type (rolled in towards the ankle). Children who are heavier. Puberty/growth spurts. External factors, e.g. hard surfaces or poor footwear. Increase in physical activity levels.
Symptoms
Typically, the sports injury occurs where the achilles tendon attaches to the bone. The epiphyseal growth plate is located at the end of a developing bone where cartilage turns into bone cells. As the growth center expands and unites, this area may become inflamed, causing severe pain when both sides of the heel are compressed. There is typically no swelling and no warmth, so it?s not always an easy condition to spot. The child usually has trouble walking, stiffness upon waking, and pain with activity that subsides during periods of rest.
Diagnosis
The doctor may order an x-ray because x-rays can confirm how mature the growth center is and if there are other sources of heel pain, such as a stress fracture or bone cyst. However, x-rays are not necessary to diagnose Sever?s disease, and it is not possible to make the diagnosis based on the x-ray alone.
Non Surgical Treatment
Treatment includes modifying activities and resting to reduce pain and inflammation and take pressure off the growth center. Ice can also be very helpful in relieving symptoms, as well as anti-inflammatory medication. A physical therapy program should be initiated to stretch tight calf muscles and strengthen the ankle muscles to relieve tension on the growth center. Shoes with padded heel surfaces and good arch support can decrease pain. Cleats may need to be avoided for some time to help reduce symptoms. The doctor may also recommend gel heel cups or supportive shoe inserts.
Achilles Tendon Injury Treatment Exercises
Overview
 Achilles tendon ruptures may be divided into full thickness ("total") and partial thickness ruptures. Total ruptures usually occur in formerly active athletes (average age 40) who resume sport activity after having been away from it for some time. In these cases, degenerative changes have weakened the tendon so much that sudden, forceful loading of the tendon causes it to tear. To some extent, these changes in the tendon could have been prevented by regular physical activity. In most cases, the injury mechanism is a strong activation of the posterior lower leg musculature, eccentrically overloading the tendon. A typical mechanism of injury involves pushing off hard with the weight-bearing foot while the knee is extended (e.g., running uphill) or sudden, unexpected dorsal extension of the ankle with reflex contraction of the calf musculature (e.g., falling down into a hole).
Achilles tendon ruptures may be divided into full thickness ("total") and partial thickness ruptures. Total ruptures usually occur in formerly active athletes (average age 40) who resume sport activity after having been away from it for some time. In these cases, degenerative changes have weakened the tendon so much that sudden, forceful loading of the tendon causes it to tear. To some extent, these changes in the tendon could have been prevented by regular physical activity. In most cases, the injury mechanism is a strong activation of the posterior lower leg musculature, eccentrically overloading the tendon. A typical mechanism of injury involves pushing off hard with the weight-bearing foot while the knee is extended (e.g., running uphill) or sudden, unexpected dorsal extension of the ankle with reflex contraction of the calf musculature (e.g., falling down into a hole).
Causes
Achilles tendon ruptures are most likely to occur in sports requiring sudden stretching, such as sprinting and racquet sports. Achilles tendon ruptures can happen to anyone, but are most likely to occur to middle age athletes who have not been training or who have been doing relatively little training. Common sporting activities related to Achilles tendon rupture include, badminton, tennis, squash. Less common sporting activities that can lead to Achilles tendon rupture include: TKD, soccer etc. Occasionally the sufferer may have a history of having had pain in the Achilles tendon in the past and was treated with steroid injection to around the tendon by a doctor. This can lead to weakening of the tendon predisposing it to complete rupture. Certain antibiotics taken by mouth or by intravenous route can weaken the Achilles tendon predisposing it to rupture. An example would be the quinolone group of antibiotics. An common example is Ciprofloxacin (or Ciprobay).
Symptoms
You may notice the symptoms come on suddenly during a sporting activity or injury. You might hear a snap or feel a sudden sharp pain when the tendon is torn. The sharp pain usually settles quickly, although there may be some aching at the back of the lower leg. After the injury, the usual symptoms are as follows. A flat-footed type of walk. You can walk and bear weight, but cannot push off the ground properly on the side where the tendon is ruptured. Inability to stand on tiptoe. If the tendon is completely torn, you may feel a gap just above the back of the heel. However, if there is bruising then the swelling may disguise the gap. If you suspect an Achilles tendon rupture, it is best to see a doctor urgently, because the tendon heals better if treated sooner rather than later.
Diagnosis
Most Achilles tendon ruptures occur in people between 30 and 50 years old and such injuries are often sport-related. If you suspect an Achilles injury, it is best to apply ice, elevate the leg, and see a specialist. One of the first things the doctor will do is evaluate your leg and ankle for swelling and discoloration. You may feel tenderness and the doctor may detect a gap where the ends of the tendon are separated. In addition to X-rays, the calf squeeze, or Thompson test, will be performed to confirm an Achilles tendon rupture. With your knee bent, the doctor will squeeze the muscles of your calf and if your tendon is intact the foot and ankle will automatically flex downward. In the case of a ruptured Achilles there will be no movement in the foot and ankle during the test.
Non Surgical Treatment
As debilitating as they can be, the good news is that minor to moderate Achilles tendon injuries should heal on their own. You just need to give them time. To speed the healing, you can try the following. Rest your leg. Avoid putting weight on your leg as best you can. You may need crutches. Ice your leg. To reduce pain and swelling, ice your injury for 20 to 30 minutes, every three to four hours for two to three days, or until the pain is gone. Compress your leg. Use an elastic bandage around the lower leg and ankle to keep down swelling. Elevate your leg. Prop you leg up on a pillow when you're sitting or lying down. Take anti-inflammatory painkillers. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) and naproxen (Aleve) will help with pain and swelling. However, these drugs have side effects, such as an increased risk of bleeding and ulcers. They should be used only occasionally unless your health care provider says otherwise and should be taken with food. Check with your doctor before taking these if you have any allergies, medical problems or take any other medication. Use a heel lift. Your health care provider may recommend that you wear an insert in your shoe while you recover. It will help protect your Achilles tendon from further stretching. Practice stretching and strengthening exercises as recommended by your health care provider. Usually, these techniques will do the trick. But in severe cases of Achilles tendon injury, you may need a cast for six to 10 weeks or even surgery to repair the tendon or remove excess tissue. 
Surgical Treatment
The procedure generally involves making an incision in the back of your lower leg and stitching the torn tendon together. Depending on the condition of the torn tissue, the repair may be reinforced with other tendons. Surgical complications can include infection and nerve damage. Infection rates are reduced in surgeries that employ smaller incisions. Rehabilitation. After treatment, whether surgical or nonsurgical, you'll go through a rehabilitation program involving physical therapy exercises to strengthen your leg muscles and Achilles tendon. Most people return to their former level of activity within four to six months.
Prevention
To prevent Achilles tendonitis or rupture, the following tips are recommended. Avoid activities that place an enormous stress on the heel (for example, uphill running or excessive jumping). Stop all activity if there is pain at the back of the heel. If pain resumes with one particular exercise, another exercise should be selected. Wear proper shoes. Gradually strengthen calf muscles with sit-ups if prior episodes of Achilles tendonitis have occurred. Always warm up with stretching exercises before any activity. Avoid high-impact sports if prior episodes of Achilles tendon injury.
Will Adult Aquired Flat Feet Always Call For Surgical Teatments ?
Overview
Have you noticed the arch in your foot collapse over a fairly short period of time as an adult? Or Do you suffer from pain on the inside and sole of your arch? If it does, then you may be suffering from a condition known as adult acquired flat foot. As one of the main support structures of the foot?s arch, the tibilais posterior tendon, along with other muscles, tendons and ligaments, play a very important role in its mechanical function. 
Causes
Adult acquired flatfoot is caused by inflammation and progressive weakening of the major tendon that it is responsible for supporting the arch of the foot. This condition will commonly be accompanied by swelling and pain on the inner portion of the foot and ankle. Adult acquired flatfoot is more common in women and overweight individuals. It can also be seen after an injury to the foot and ankle. If left untreated the problem may result in a vicious cycle, as the foot becomes flatter the tendon supporting the arch structure becomes weaker and more and more stretched out. As the tendon becomes weaker, the foot structure becomes progressively flatter. Early detection and treatment is key, as this condition can lead to chronic swelling and pain.
Symptoms
The first stage represents inflammation and symptoms originating from an irritated posterior tibial tendon, which is still functional. Stage two is characterized by a change in the alignment of the foot noted on observation while standing (see above photos). The deformity is supple meaning the foot is freely movable and a ?normal? position can be restored by the examiner. Stage two is also associated with the inability to perform a single-leg heel rise. The third stage is dysfunction of the posterior tibial tendon is a flatfoot deformity that becomes stiff because of arthritis. Prolonged deformity causes irritation to the involved joints resulting in arthritis. The fourth phase is a flatfoot deformity either supple (stage two) or stiff (stage 3) with involvement of the ankle joint. This occurs when the deltoid ligament, the major supporting structure on the inside of the ankle, fails to provide support. The ankle becomes unstable and will demonstrate a tilted appearance on X-ray. Failure of the deltoid ligament results from an inward displacement of the weight bearing forces. When prolonged, this change can lead to ankle arthritis. The vast majority of patients with acquired adult flatfoot deformity are stage 2 by the time they seek treatment from a physician.
Diagnosis
Your podiatrist is very familiar with tendons that have just about had enough, and will likely be able to diagnose this condition by performing a physical exam of your foot. He or she will probably examine the area visually and by feel, will inquire about your medical history (including past pain or injuries), and may also observe your feet as you walk. You may also be asked to attempt standing on your toes. This may be done by having you lift your ?good? foot (the one without the complaining tendon) off the ground, standing only on your problem foot. (You may be instructed to place your hands against the wall to help with balance.) Then, your podiatrist will ask you to try to go up on your toes on the bad foot. If you have difficulty doing so, it may indicate a problem with your posterior tibial tendon. Some imaging technology may be used to diagnose this condition, although it?s more likely the doctor will rely primarily on a physical exam. However, he or she may order scans such as an MRI or CT scan to look at your foot?s interior, and X-rays might also be helpful in a diagnosis.
Non surgical Treatment
Treatment will vary depending on the degree of your symptoms. Generally, we would use a combination of rest, immobilization, orthotics, braces, and physical therapy to start. The goal is to keep swelling and inflammation under control and limit the stress on the tendon while it heals. Avoidance of activities that stress the tendon will be necessary. Once the tendon heals and you resume activity, physical therapy will further strengthen the injured tendon and help restore flexibility. Surgery may be necessary if the tendon is torn or does not respond to these conservative treatment methods. Your posterior tibial tendon is vital for normal walking. When it is injured in any way, you risk losing independence and mobility. Keep your foot health a top priority and address any pain or problems quickly. Even minor symptoms could progress into chronic problems, so don?t ignore your foot pain. 
Surgical Treatment
A new type of surgery has been developed in which surgeons can re-construct the flat foot deformity and also the deltoid ligament using a tendon called the peroneus longus. A person is able to function fully without use of the peroneus longus but they can also be taken from deceased donors if needed. The new surgery was performed on four men and one woman. An improved alignment of the ankle was still evident nine years later, and all had good mobility 8 to 10 years after the surgery. None had developed arthritis.